What is Nail Intramedullari and How Does it Work?
nail intramedullari has revolutionized orthopedic surgery in recent years. It serves as a crucial component for treating fractures, particularly in long bones. According to a 2022 report by the Orthopedic Research Society, the global market for Nail Intramedullari devices is expected to see an annual growth rate of 7.4%. This indicates a rising reliance on this technique among surgeons.
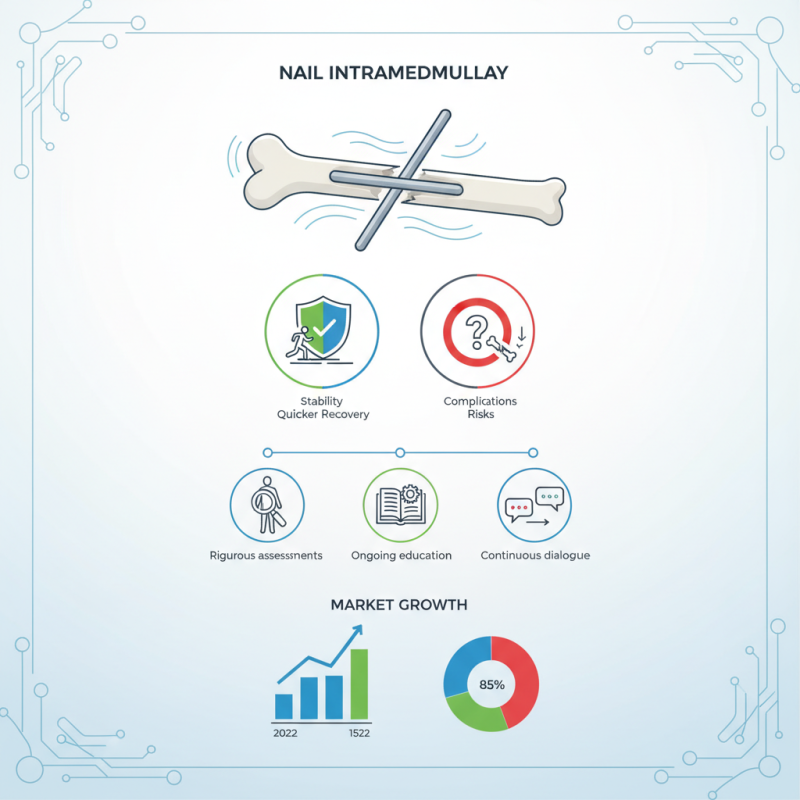
Dr. Lisa Thompson, a leading expert in orthopedic surgery, noted, "Nail Intramedullari offers excellent stability and facilitates quicker recovery for patients." Yet, while many surgeries yield positive outcomes, some still face complications. The challenge lies in determining the right candidate for these procedures. Statistics reveal that 15% of patients experience complications, emphasizing the need for rigorous assessments prior to implementation. Moreover, as more surgeons adopt this technique, ongoing education becomes vital to understanding its limitations and potential risks.
In conclusion, the impact of Nail Intramedullari is vast, but it warrants careful consideration. As this field evolves, continuous dialogue among medical professionals will be essential.
What is Nail Intramedullari?
Nail intramedullari is a surgical technique used to treat bone fractures. It is particularly effective for long bones, like the femur or tibia. The method involves inserting a metal rod into the marrow cavity of the bone. By providing internal support, it helps stabilize the fracture during the healing process.
During the procedure, a small incision is made at the fracture site. The surgeon carefully navigates the rod into the bone. This process requires precision and expertise. Post-surgery, patients may experience discomfort and a lengthy recovery. Some may struggle with mobility, and the healing time can vary significantly. Individuals often have questions about their progress and the effectiveness of the procedure.
While nail intramedullari is largely successful, it is not without complications. Infections and malalignment can occur. Patients may need additional surgeries to correct these issues. Furthermore, the psychological impact of such procedures is sometimes overlooked. Understanding the procedure can help manage expectations and encourage patience during recovery.
Nail Intramedullari Usage Statistics
This chart illustrates the distribution of nail intramedullari usage in various orthopedic procedures over the past year.
History and Development of Intramedullary Nails
Intramedullary nails have a significant history in the field of orthopedic surgery. They emerged in the mid-20th century as a solution for long bone fractures. Initially developed for their structural advantages, these nails allow for minimal soft tissue damage during insertion. The design of these nails has changed steadily over the years. Early models were often bulky and less effective. Today, advanced materials like titanium enhance strength while reducing weight.
Researchers and engineers have continually refined intramedullary nails. In the 1980s and 1990s, the focus shifted towards better alignment and stabilization. This transformation aimed to improve patient outcomes. Various designs suited different types of fractures emerged. However, not every nail has been a success. Some designs faced complications, leaving surgeons to reconsider approaches.
Medical professionals often encounter challenges with intramedullary nails. Incorrect placement can lead to non-union or improper healing. Surgeons must stay updated on evolving techniques. Training and experience play crucial roles in maximizing the benefits of intramedullary nailing. Recognition of these challenges is essential for progress in surgical practices.
Indications for Using Intramedullary Nails in Surgery
Intramedullary nails are a surgical tool used to stabilize broken bones. Surgeons often choose this method for various reasons. It is particularly useful for long bone fractures. These include femur, tibia, and humerus. Intramedullary nailing allows for better alignment and stability. This is crucial for proper healing.
One key indication for using intramedullary nails is when fracture fixation is challenging. Fractures that are unstable or have multiple fragments may require this technique. Intramedullary nails can adapt to different shapes and sizes of bones. Surgeons appreciate this versatility in complex cases. Additionally, it helps patients regain mobility faster compared to other methods.
**Tips:** Before opting for this treatment, consult with a medical professional. They will assess your unique case and determine suitability. It’s important to ask questions about potential complications. Understanding the risks can help you make an informed decision. Listening to your doctor's advice can also enhance recovery.
What is Nail Intramedullari and How Does it Work? - Indications for Using Intramedullary Nails in Surgery
| Indication | Description | Common Procedures |
|---|---|---|
| Femoral Fractures | Intramedullary nails provide stabilization for fractured femurs by being inserted into the medullary cavity. | Closed or open reduction, nail insertion through suprapatellar or infrapatellar routes. |
| Tibial Fractures | Used in the management of both shaft and distal fractures of the tibia to promote healing. | Nailing from the proximal or distal ends based on fracture location. |
| Humeral Fractures | Intramedullary fixation is employed for humeral shaft fractures offering robust stabilization. | Retrograde nailing, often involving a deltopectoral approach. |
| Non-Union or Malunion | Indicated when previous fractures have not healed properly, providing needed support and alignment. | Revision nailing or augmenting fixation with additional procedures. |
| Osteogenesis Imperfecta | Used in pediatric patients to stabilize fractures due to brittle bone conditions. | Insertion of flexible intramedullary nails in children. |
The Surgical Procedure for Intramedullary Nailing
Intramedullary nailing is a common surgical procedure for treating fractures. It involves inserting a rod into the medullary cavity of a bone. This technique stabilizes fractures, particularly in long bones like the femur and tibia. Studies show that intramedullary nailing can reduce healing time by approximately 20%. It allows for early mobilization, which is vital for recovery.
The surgical procedure begins with anesthesia. The surgeon makes an incision to access the bone. A guide wire is then inserted into the medullary canal, serving as a pathway for the nail. Intramedullary nails come in various sizes. They must be selected carefully to match the patient's anatomy. Research indicates that about 10% of patients may experience complications, such as infection or misalignment.
Post-operative recovery is critical. Patients often start rehabilitation within days. Physical therapy helps regain strength and mobility. However, some individuals may struggle with pain management and adherence to rehabilitation protocols. These factors can affect overall recovery. Monitoring progress for potential complications is crucial, as early intervention can make a difference.
Benefits and Risks of Nail Intramedullari in Bone Fractures
Nail intramedullari is a technique for treating bone fractures. It involves inserting a metal rod into the bone marrow. This procedure stabilizes the fracture and allows for better healing. Many surgeons prefer this method due to its minimally invasive nature.
The benefits of nail intramedullari include faster recovery times and less trauma to surrounding tissues. Patients often experience less pain post-surgery compared to traditional fixation methods. This technique can also lead to a lower risk of infection. However, there are risks. Misalignment during the procedure can occur, potentially leading to complications. Some patients report discomfort from the metal rod, which may require a follow-up procedure for removal.
Understanding the benefits and risks is crucial. Nail intramedullari may not be suitable for all fractures. An accurate diagnosis is necessary for optimal outcomes. Patients should discuss their options with their surgeon. This decision is significant and can profoundly impact recovery and long-term mobility.
